A Close Look at How COVID-19 Infection Can Damage the Brain
A Close Look at How COVID-19 Infection Can Damage the Brain
In a much-discussed report appearing online March 26 in the Journal of the American Medical Association (JAMA), three researchers have attempted to explain the potential causes of a wide range of neuropsychiatric symptoms seen in some patients infected with the COVID-19 virus.
In addition to anosmia—a loss of the sense of smell commonly reported by COVID-19 patients and therefore linked to the brain's olfactory processing system—the researchers note a range of other reported neuropsychiatric symptoms. These include cognitive and attention deficits ("brain fog"), new-onset anxiety, depression, psychosis, seizures, and suicidal behavior.
These have been present in patients before, during, and after the respiratory symptoms caused by COIVD infection, the researchers note, and "are unrelated to respiratory insufficiency." Rather, they say, these brain and behavior symptoms "suggest independent brain damage" attributable to COVID-19 infection.
The researchers include the report's lead author, Maura Boldrini, M.D., a 2014 BBRF Independent Investigator and 2006 and 2003 Young Investigator at the New York State Psychiatric Institute and Columbia University. Dr. Boldrini, a neuropathologist and psychiatrist, was joined by Peter Carroll, M.D., Ph.D., a pathologist and cell biologist also at Columbia, and Robyn Klein, M.D., Ph.D., an expert in pathology, immunology, and neuroscience at Washington University St. Louis.
Information about COVID-19's impact on the brain is preliminary. Patient follow-ups conducted in Germany and the UK found post-COVID neuropsychiatric symptoms in 20% to 70% of patients—a very wide range reflecting their still uncertain prevalence. The symptoms were seen in young adults as well as older adults, and in some instances lasted months after the resolution of respiratory symptoms. This evidence suggests to the researchers that "brain involvement" due to COVID-19 persists in many cases.
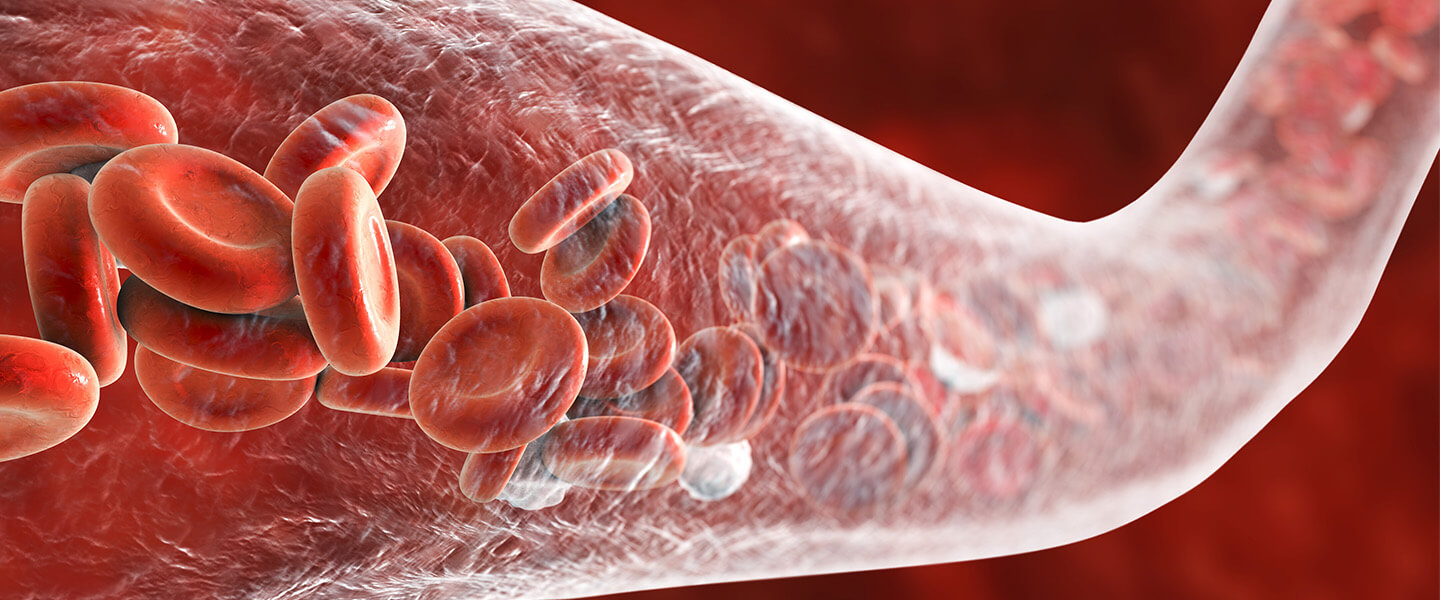
In search of biological processes which may be interrupted by COVID-19, the researchers begin with the virus' entry into the body, thought frequently to occur at cellular docking ports called ACE2 receptors found in cells of the lungs and arteries (as well as in the heart, kidneys, and intestines). The virus can damage endothelial cells that line blood vessels and arteries. This, the researchers note, can cause inflammation, the formation of blood clots (thrombi), and lead to brain damage.
When inflammation becomes systematic in the body, it can have many effects. Among these are decreased production of monoamines and trophic factors—proteins in the brain involved in neurotransmission and maintenance of neuronal growth.
Inflammation also leads to the activation of microgila. These are the immune cells unique to the brain and spinal cord which have the crucial role of removing plaque-like build-ups in the central nervous system (CNS) as well as removing damaged or unnecessary neurons and synaptic connections. Substantial reduction in microglia numbers is associated with increased activity of the excitatory neurotransmitters glutamate and NMDA, sometimes resulting in what scientists call excitotoxicity, a kind of damage caused by overactivation of excitatory neurons and their receptors.
The researchers note that COVID-19 proteins have been found in the lining of blood vessels in the brain. While evidence is still lacking as to whether COVID-19 actually infects the brain, the researchers note various means by which viral particles might leak through the blood-brain barrier (BBB), a membrane that is designed to protect the brain from viruses, toxins, and other harmful factors.
The researchers speculate that loss of the sense of smell as well as nausea and vomiting may be related to viral invasion of brain and CNS vasculature, and they suggest that other short- and long-term neuropsychiatric symptoms "are more likely due to neuroinflammation and hypoxic injury [deficiency of oxygen due to interruption of blood flow in the brain]." COVID-19 infiltration of the brain stem, they add, may be involved in problems with the autonomic nervous system (which controls heart rate, respiration, digestion, etc.) as well as in anxiety symptoms reported by COVID-19 patients.
In explaining other impacts of the virus upon the brain and CNS, the researchers note that when the virus enters the endothelial cells lining the blood vessels of the brain, cells called neutrophils and macrophages are activated, and thrombins are produced. These are among the factors leading to the production of "microthrombi" within blood vessels—tiny clots. "Neuropsychiatric symptoms of COVID-19 could result from micro-strokes and neuronal damage," they say, with the specific symptoms varying in patients according to where in the brain or spinal cord such events occur.
In fact, the researchers suggest, mechanisms involved in COVID-19 brain damage "may resemble those involved in traumatic brain injury." In such injuries, like those seen in some football players, inflammation and injury to blood vessels in the brain resulting in the loss of neurons have been implicated in pathology that gives rise to suicidal behavior. Understanding COVID-related brain injury may provide insights for research on traumatic brain injuries, they note.
Pathologies induced by COVID-19, as best they can be deduced now, suggest to the team a variety of potential interventions to lessen their impact. These include: administering agents which suppress cytokines, the immune-signaling molecules involved in generating the "cytokine storm" associated with pathology in severe COVID-19 cases; administering agents such as ketamine which suppress NMDA receptors; and administering agents such as aspirin and celecoxib (Celebrex) which have an anti-inflammatory effect.



