A Problem With Energy-Producing Mitochondria May Increase Risk for Schizophrenia
A Problem With Energy-Producing Mitochondria May Increase Risk for Schizophrenia
One of the most important objectives in brain research is to understand in detail how genetic abnormalities impact the ability of brain cells and circuits to function properly. This is one of the keys to unlocking the mysteries of causation in a range of psychiatric illnesses, especially those thought to have a strong genetic component. Among these are neurodevelopmental disorders such as schizophrenia and autism spectrum disorder (ASD) in which contributing pathology is thought to occur at the dawn of life.
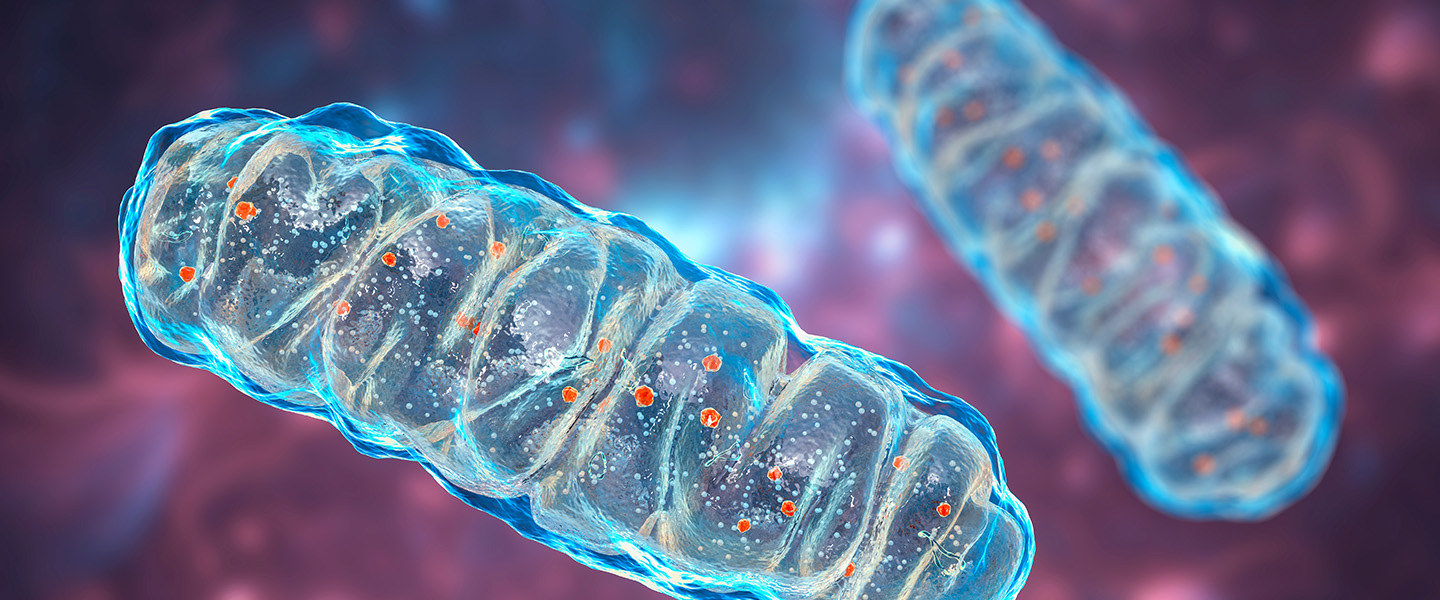
A newly published study appearing in Science Advances, whose authors include six current and past BBRF grantees, makes an important contribution to this effort, giving the research community reason to consider a factor not currently at the focus of schizophrenia research: the tiny energy factories called mitochondria that are present in large numbers in every brain cell.
A team of collaborating researchers from Emory and Rutgers universities proposed to learn something of potentially broad significance about schizophrenia causation by studying, paradoxically, one of the rarest known genetic mutations associated with the illness. Called 3q29 deletion syndrome, it is believed to occur in about 1 in 30,000 people; it also has the distinction of being the most powerful risk factor for schizophrenia currently known: those with the syndrome—they are missing a segment of chromosome 3—have a 40-fold increase in risk of developing schizophrenia. The syndrome also is linked with intellectual disability, ASD, and ADHD, among other illnesses.
The question addressed by the team was how, precisely, the genetic deletion that causes 3q29 deletion syndrome affects the functioning of cells in the brain; and how these impacts might contribute to causation in schizophrenia. Although 3q29 deletion syndrome is rare, the team reasoned that by restricting their investigation to the single genome variation that causes it, they would be able to search for impacts directly attributable to it and not to the plethora of other factors, including other genetic variations, that have been implicated in other schizophrenia studies over the years.
The team was co-led by Jennifer G. Mulle, Ph.D., a 2007 BBRF Young Investigator, and Gary J. Bassell, Ph.D., a 2012 BBRF Distinguished Investigator and 2009 Independent Investigator. Co-first author of the team’s paper was Ryan H. Purcell, Ph.D., whose 2021 BBRF Young Investigator grant funded some of the research that led to the new paper. The other co-first author was Esra Sefik, Ph.D. Bonnie L. Firestein, Ph.D., a 2012 BBRF Distinguished Investigator and 2007 Independent Investigator; Steven A. Sloan, M.D., Ph.D., a 2019 BBRF Young Investigator; and Nisha Raj, Ph.D., a 2022 BBRF Young Investigator, were also members of the team.
“For genetic variants associated with schizophrenia, we want to understand the primary pathology at the cellular level,” noted Dr. Purcell. “This gives us a foothold which may help cut through schizophrenia’s complexity and better understand the neurobiology.”
The team used two experimental systems as the basis for their observations. One was a mouse model in which the 3q29 region was snipped out in each individual mouse using CRIPSR gene-editing technology. This model had been developed and tested previously, and provided the team with a source of brain tissue containing cells presumably perturbed by the mutation. The mouse brains were studied 7 days after birth, a time corresponding with early human development.
The second experimental model came from brain cells affected by the deletion that were gown in culture dishes in the lab, using a revolutionary technology made possible by stem cell biology. Called hiPSC (human induced pluripotent stem cell) technology, it enables researchers to harmlessly sample cells from human subjects (in this case, blood cells) and reprogram them in the lab to re-develop, in these experiments, as brain cells. The cells carry the full genome of the donor. Reprogrammed, they grow in lab dishes and form living, functioning clumps called organoids, and are quite similar in many respects to human cells at the beginning of life. In this case, different collections of these reprogrammed cells were studied after growing for 2 months and 12 months in the dish. It was later confirmed that their identity and activity most closely resembled human cells in the first and second trimesters of gestation. Cells for these organoids were sampled from patients with 3q29 deletion syndrome as well as healthy individuals; some of the latter, after reprogramming, were genetically engineered using CRISPR to carry the 3q29 deletion.
The team carefully analyzed patterns of gene expression in the different sets of brain cells carrying the 3q29 deletion, and in so doing reported they had “isolated the effects of 3q29 deletion in the developing cerebral cortex.” Dr. Mulle commented: “Our data give strong support to the hypothesis that mitochondrial dysregulation is a contributor to the development of schizophrenia.” It was Dr. Mulle and colleagues who, in 2010, first showed that 3q29 deletion was a risk factor for schizophrenia. Dr. Mulle’s 2007 BBRF Young Investigator Award helped drive this initial discovery.
The 3q29 deletion covers an area occupied by 22 human genes. By looking in the brain cells making up the organoids, as well as the cells sampled from the cortex in affected mice, the team zeroed in on the “transcripts” of these genes—readouts of their activation patterns. The altered patterns, relative to the transcripts in cells from healthy people very early in life, suggested that genetic changes affect the ability of cortical cells to adapt adequately to energy-related challenges—they lacked “metabolic flexibility.”
How this lack of flexibility might contribute to pathology that causes schizophrenia remains conjecture, although the new study will likely spur additional research. It is possible that a popular theory of schizophrenia causation—that genetic variations combine to affect the formation and operation of synapses, the trillions of connection points that enable neurons throughout the brain to communicate—is not inconsistent with the new discovery about possible mitochondrial pathology. Neurons need lots of energy to build and maintain synapses, including at the beginning of life as the brain wires up. A deficit in cellular energy production might contribute to problems establishing or maintaining synapses.
Another rare genetic syndrome that greatly raises risk for schizophrenia called 22q11.2 deletion syndrome (caused by a genetic deletion on chromosome 22) is known to affect eight genes that encode proteins found in mitochondria. Other research has demonstrated that the 22q11.2 deletion also impacts the function of mitochondria. These two rare syndromes, therefore, have given researchers new reason to further investigate the possible involvement of mitochondria in schizophrenia causation—whether or not future research confirms or disproves a connection with synaptic formation and function.
The overall aim of “bridging the gap between genetic risk and [dysfunction] in biological mechanisms is a major challenge for psychiatry,” the team noted in its paper. To this end, Dr. Purcell is now conducting a study designed to determine whether cells from people with 22q11.2 deletion display the metabolic instability seen in the 3q29 deletion study.





