A New Approach to Treating Cognitive Deficits in Schizophrenia
Dr. Vikaas Sohal used a new technology to understand why cognition is impaired in schizophrenia and now is exploring how it might be targeted.
Vikaas S. Sohal, M.D., Ph.D.
Associate Professor, Psychiatry UCSF Weill Institute for Neurosciences
University of California, San Francisco
BBRF Scientific Council Member
2009 Young Investigator Grant
Decades of observation and experiment have established that cognitive deficits are among the core features of schizophrenia. As one recent paper on the subject notes: “Studies have shown that compared to healthy controls, schizophrenia patients have impaired cognitive performance across all cognitive domains including processing speed, attention and vigilance, working memory, verbal learning, visual learning, reasoning/problem solving, and social cognition.”
Patients find it difficult to focus or concentrate; to organize their thoughts; to keep newly acquired information “in mind”; to modify or adapt their behavior in response to new sounds and sights; to make sense of perplexing experiences or unfamiliar information.
These cognitive difficulties directly affect the ability to get along in society. Resulting problems in social functioning can lead to social isolation, and to interpersonal problems which can exacerbate symptoms and thus significantly impair quality of life, interfering with rehabilitation or efforts to get and keep a job.
All of this is well known. But one thing is not often said: no one really understands why cognitive dysfunction occurs in people with schizophrenia.
Cognitive impairment is the “major cause of disability” in schizophrenia, and helps explain why the illness remains stubbornly disabling for many patients, according to BBRF Scientific Council member Vikaas S. Sohal, M.D., Ph.D.
A practicing psychiatrist and a leading neuroscience researcher, with a lab at the University of California, San Francisco (UCSF), Dr. Sohal notes that antipsychotic medicines, which are essential tools in managing psychotic symptoms such as hallucinations and delusions, don’t address cognitive impairment. And while many cognitive remediation treatment strategies have been tested and have helped some patients, their effectiveness varies, he says. Like antipsychotic medicines, “they have not really been developed on the basis of understanding the biological mechanisms that actually cause cognitive deficits.”
Thanks to a new technology that was emerging just as Dr. Sohal completed his training—developed in part with help from BBRF grants—and to experiments performed with that and other advanced technologies, he and his colleagues in recent years have made discoveries that have revealed, at last, biological processes that are likely involved in causing cognitive dysfunction.
In an “Overview” paper he published in April 2022 in the American Journal of Psychiatry, Dr. Sohal suggested how this new knowledge might be translated in the coming years into new treatments for cognitive deficits in schizophrenia.
‘RIGHT PLACE, RIGHT TIME’
Dr. Sohal’s highly productive research career, still in its early stages, exemplifies how investments in basic research and in the development of new technologies can pay great dividends in ways that cannot possibly be predicted in advance. Apart from his academic brilliance—he studied Applied Mathematics at Harvard as an undergrad, Mathematics at the University of Cambridge, UK, and then went on to complete an M.D.- Ph.D. program at Stanford University in 2005—Dr. Sohal’s early orientation as a neuroscientist did not indicate a particular focus on cognitive deficits in schizophrenia.
His early career parallels that of one of his mentors, Dr. Karl Deisseroth, who preceded him in the Stanford M.D.-Ph.D. program by a few years. Last year, Dr. Deisseroth received the highly prestigious Lasker Basic Medical Research Award, sharing it with two others who helped develop optogenetics. In essence, optogenetics enables experimenters to switch specific neurons, or groups of them, “on” and “off,” doing so with beams of colored light directly conducted into the brain via optical fibers no wider than a thread.
Dr. Deisseroth received BBRF Young Investigator awards in 2005 and 2007, which helped support him as he was setting up his Stanford lab where some of the earliest optogenetics research was conducted. This is when he and Dr. Sohal met. “When I graduated [the Stanford M.D.-Ph.D. program], Karl had just finished his [medical] residency and was starting his lab,” Dr. Sohal remembers. “It was an example of being at the right place, at the right time. We got along, and he was interested in the same general things that I was. I was able to join his lab, before returning to my own residency and then starting my own lab after that.”
Just as Dr. Deisseroth had received early-career support from BBRF, so did Dr. Sohal, when he finished his medical residency and began his own research program. His Young Investigator award was made in 2009, and by 2017 his accomplishments merited his election to BBRF’s Scientific Council—just as Dr. Deisseroth’s had in 2008, at a similarly early point in his career.
When Dr. Sohal says he and Dr. Deisseroth shared research interests, he means a passion for understanding mechanisms in the brain, at the level of cells and the complex circuits they form. In ways that until very recently have been a black box, brain cells and circuits give rise to astonishing properties such as memory, the ability to learn, and that ultimate miracle and mystery, consciousness itself.
Like many other contemporary researchers, Drs. Deisseroth and Sohal have made it their life’s work to devise ways to study the brain at the cellular and circuit level while it is operating, in living beings, and to use these technologies to begin to unpack how, for example, circuits appear to function differently when someone has major depressive disorder or obsessivecompulsive disorder, or, indeed, schizophrenia. The road to bold new treatments is being paved with this knowledge.
OPTOGENETICS UNRAVELS A MYSTERY
A major milestone in the careers of these colleagues occurred while Dr. Sohal was working in Dr. Deisseroth’s Stanford lab. These were the years in which optogenetics, with its stunning capability of controlling specific neurons and circuits, was put to a test. These early experiments were opportunities to show how the new technology could not only reveal something previously unknowable about how the brain works, but also how brain biology might be perturbed in mental illness.
In 2008 and 2009, Drs. Sohal and Deisseroth used optogenetics to test the validity of a theory that until then was impossible to prove or disprove. They were interested in a subclass of neurons: neurons that release the inhibitory neurotransmitter GABA. These specialized cells reduce or suppress neural signaling. They sit in the middle of local brain circuits composed mostly of excitatory neurons. The brain’s proper functioning vitally depends upon them. Without properly functioning inhibitory cells, circuits can overload with excitation, resulting in seizures.
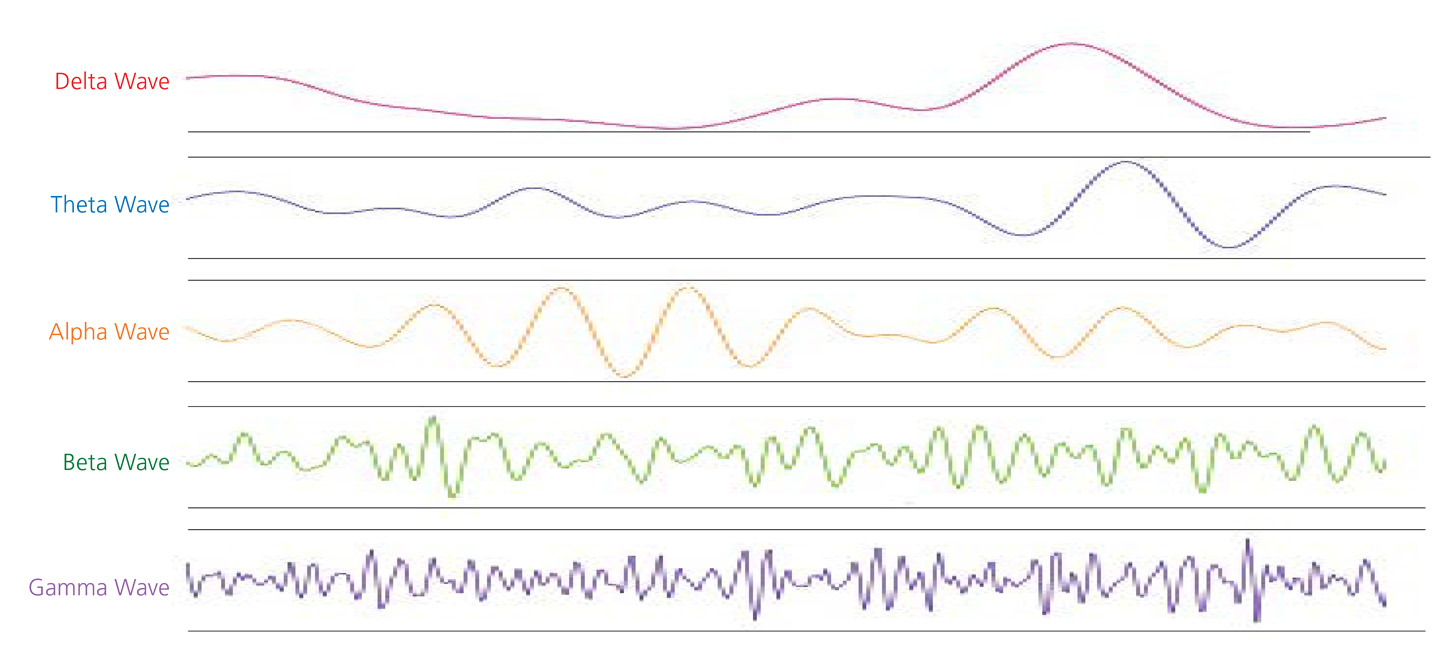
Drs. Deisseroth, Sohal and colleagues focused on a subtype of inhibitory cells called PV interneurons, named for a protein (parvalbumin) that they express which distinguishes them from other inhibitory cell types. PV interneurons make up about 40 percent of inhibitory neurons in the cerebral cortex, seat of the brain’s higher functions. There had been speculation that they played an essential role in enhancing information processing; they were thought to be associated with a kind of rhythmic activity in the brain called gamma oscillations. There are irregularities in gamma oscillations in people with schizophrenia. But until optogenetics, there was no precise way of proving how PV interneurons affected gamma oscillations, and in turn, how gamma oscillation irregularities might impair information processing in schizophrenia—a potential clue to explain cognitive deficits.
The team used optogenetics to switch off PV interneurons in part of the rodent cortex. This provided direct evidence that inhibiting these inhibitory cells reduced gamma oscillations. In related experiments, the team stimulated PV interneurons in the rodent brain, and found that this not only increased gamma oscillations, but tended to establish a gammafrequency rhythm. This rhythm was the result of synchronized activity between excitatory and inhibitory cells within the circuit being studied. Perhaps most intriguing, the team was able to show that when a gamma rhythm was established, signal transmission was enhanced: “noise” in the circuit (useless information) was reduced, and the important “signal” carried by the circuit was enhanced.
These experimental results, reported in Nature in 2009, helped establish the utility of optogenetics, which is now a staple research tool in labs around the world. They also help to explain important aspects of the career that Dr. Sohal was just embarking upon, which has since blossomed in many directions. One unifying feature is his consistent fascination with systems composed of relatively simple parts, which, when functioning together, give rise to what are called emergent properties. The early experiments with PV interneurons provided a wonderful example: when these inhibitory cells were spurred, using optogenetics, they promoted a “gamma rhythm” across the circuit, which enabled the rodent brain to process information more efficiently.
Neural rhythms turn out to be very important in understanding how the brain works, and while Dr. Sohal has performed research involving other frequencies of neural oscillations, the gamma frequency, which captures fast neural oscillations (each cycle lasting 10 to 30 thousandths of a second) has turned out to have important implications for understanding cognitive dysfunction in schizophrenia.
Like most research, Dr. Sohal’s has built upon prior clues. By studying postmortem brain tissue, other researchers had learned that various kinds of pathologies involving PV interneurons are commonplace in people with schizophrenia. BBRF Scientific Council Member, 2008 Distinguished Investigator, and 2005 Lieber Prize winner David A. Lewis, M.D., of the University of Pittsburgh, has led studies in schizophrenia patients revealing deficits in the ability of cortical circuits to generate gamma-frequency activity. Some scientists have speculated that irregularities in gamma-frequency activity are a precursor of a first psychotic episode—typically, the event which immediately precedes the onset of schizophrenia.
Yet there is a pivotal question about these gamma-frequency clues. As Dr. Sohal put it in his recent “Overview” paper: “Do gamma oscillations simply indicate that brain circuits are active— akin to the roar of a car’s V8 engine— or do they actually perform functions that enhance the performance of brain circuits?” There was a suggestion of the latter in the 2009 paper. But additional research was needed to know more.
In 2015 and 2020, Dr. Sohal’s team published papers, respectively, in Neuron and Nature Neuroscience, describing experiments which shed new light on this question—mouse studies that gave direct evidence that gamma oscillations aren’t just the “sound” of the brain doing its job, but actually contribute to cognition. The experiments also suggested that restoring normal gamma-frequency activity in the cortex might reduce or even reverse the kind of cognitive deficits seen in schizophrenia.
In the 2015 paper, experiments were led by Kathleen K.A. Cho, Ph.D., a 2013 BBRF Young Investigator who studies and works with Dr. Sohal and John Rubenstein, M.D., Ph.D., a three-time BBRF grantee, 2016 BBRF Ruane Prize winner and emeritus Scientific Council member who is also at UCSF.
The team worked with mice that were bred with deficiencies in PV interneurons. These mice develop deficits in cognitive flexibility, a trait that is impaired in schizophrenia. Like normal mice, the mutant mice were able to learn a rule governing a particular task; but unlike the normal mice, those with PV interneuron abnormalities were unable to adapt when the rules were shifted. They “perseverated” in their behavior— kept going back to the rule they learned initially even though it was no longer effective.
REVERSING COGNITIVE DEFICITS
Two fascinating things emerged from this. First, it was shown that when normal mice learned the “new” rule, gamma oscillations in the prefrontal cortex were increased, while in the mutant mice, they were deficient. Second: when the team used optogenetics to increase gamma oscillations in the cortex of the mutant mice, they were then able to learn the new rule and obtain a reward. And this ability persisted over a period of weeks: the corrective was long-lasting in its effect. “Performance was completely normalized,” Dr. Sohal comments. This suggested—but did not prove—that certain cognitive deficits in schizophrenia might likewise be reversed, at least in principle.
The second paper, of 2020, put the same team to work on discovering why the enhancement of gamma oscillations was effective in boosting cognitive capacity. This time, key experiments were performed in normal mice. The researchers looked at what happened in PV interneurons when the mice were in the process of learning a new rule. This revealed the importance of what Drs. Sohal, Cho and colleagues call gamma synchrony. Not only did cortical gamma oscillation levels increase when a new rule was learned; in fact, oscillations became synchronized across the brain’s two hemispheres. Optogenetics was used to disrupt this cognition-boosting synchrony. Doing so prevented the mice from learning the new rule. Restoring synchrony restored the animals’ ability to learn the new rule.
Speaking about this experiment today, Dr. Sohal, after prompting, conceded that it was indeed a “wow” result. “But remember,” he added, with the caution that characterizes most scientists, “We are talking about mice, not people.”
Although research in the Sohal lab is wide-ranging and has potential relevance for many psychiatric illnesses, the line of work on gamma oscillations has implications that Dr. Sohal has now explained in some detail to the psychiatric community. In his recent “Overview” paper he explains that there are, in principle, a number of ways to enhance gamma synchrony in the human brain.
While optogenetics can establish gamma synchrony in mice, it can only be used, ethically, in laboratory animals, since it involves brain surgery. In humans, gamma oscillations might be altered with a number of pharmaceutical compounds, Dr. Sohal says, for instance “low doses or welltitrated doses of benzodiazepines [anti-anxiety agents] or drugs like clonazepam or lorazepam, which are commonly used at higher dosages to sedate people.” But these drugs have actions that are not specific to PV interneurons and may have unwanted side effects.
It is possible, Dr. Sohal says, that current pharmaceutical technology can support the development of agents that specifically target a subset of cellular receptors for GABA, the neurotransmitter that is released by PV interneurons. The idea would be to selectively modulate the action of PV interneurons, as a way of addressing gamma oscillation and promoting gamma synchrony.
Another possibility is being explored by Cameron Carter, M.D., of UC Davis, who is also a BBRF Scientific Council member as well as 2-time BBRF grantee and winner of the BBRF Klerman Prize. As Dr. Sohal notes, Dr. Carter is exploring the use of non-invasive brain stimulation—tDCS (transcranial direct current stimulation)—to alter gamma oscillations as a possible way of addressing cognitive dysfunction.
A number of questions remain before these treatment approaches can be tested in healthy people and then in patients with cognitive dysfunction. If drugs are to be used, it will be important to understand what they target in the brain and what their offtarget effects might be; what doses to use and how to predict which patients might benefit and which might not.
Dr. Sohal also says it will be of great value to know more about where and when to boost gamma activity. Circuits in the cortex are famously complex, consisting of many different types and subtypes of both excitatory and inhibitory neurons. Are there specific places, even specific synapses, in the brain to target to boost gamma activity and cognition? Or should large areas be targeted? Should treatments be continuous or need they be given only occasionally or rarely or even just once? All of these questions and many others remain to be explored in the next several years before it is reasonable to test these concepts in people.
Yet Dr. Sohal is hopeful. In his recent “Overview” paper, he wrote: “It is now clear that gamma synchronization contributes to the function of brain circuits in ways that could be highly relevant for treating cognitive deficits in condition such as schizophrenia. In fact, the complexity of cortical microcircuits may turn out to be a major asset, not a barrier, by enabling us to target particular aspects of gamma synchrony in a relatively specific manner.”
Elsewhere he adds: “There is no reason to assume that interventions should be limited to pharmacology. It might be possible to administer a drug that enhances the capacity for a circuit to generate gamma synchrony in concert with a behavioral intervention such as cognitive training, meditation, or biofeedback, or noninvasive brain stimulation (e.g. tDCS) to enhance gamma oscillations.”
Written By Peter Tarr, Ph.D.
Click here to read the Brain & Behavior Magazine's December 2022 issue